What is **Leptospirosis**?
Creator: Gilnature | Credit: Getty Images
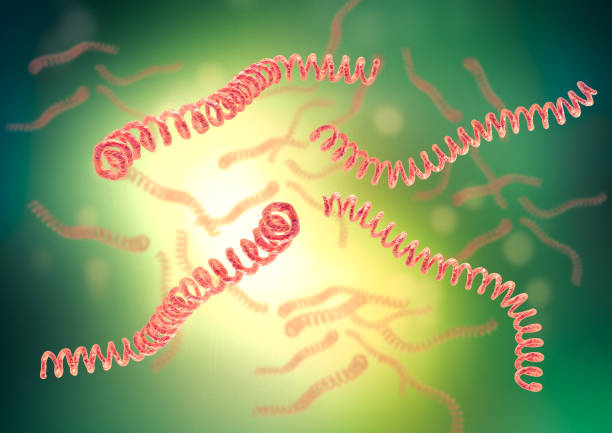
Leptospirosis is a bacterial disease that affects humans and animals. It is caused by bacteria of the genus Leptospira. Here’s a comprehensive overview of the disease:
Etiology
Causative Agent: Leptospira spp., which are spiral-shaped bacteria.
Reservoirs: Wild and domestic animals, particularly rodents, which are the primary reservoirs. Other animals like dogs, cattle, pigs, and horses can also carry the bacteria.
Transmission
Direct Contact: Through the urine of infected animals or through contact with water, soil, or food contaminated with urine.
Routes of Entry: The bacteria enter the body through cuts or abrasions on the skin, mucous membranes (eyes, nose, mouth), or through ingestion of contaminated water or food.
Epidemiology
Geographic Distribution: Worldwide, more common in tropical and subtropical regions.
Risk Factors: Occupations involving animal handling (farmers, veterinarians), recreational activities (swimming in contaminated water), and natural disasters (floods).
Pathophysiology
After entry, Leptospira disseminates through the bloodstream and can affect multiple organs, including the liver, kidneys, lungs, and central nervous system.
Clinical Manifestations
Leptospirosis has a wide range of symptoms, often divided into two phases:
Acute (Leptospiremic) Phase:
Incubation Period: 2-30 days (commonly 5-14 days).
Symptoms: Sudden onset of fever, chills, headache, muscle pain, vomiting, jaundice, red eyes, abdominal pain, diarrhea, and rash.
Immune (Leptospiruric) Phase:
Symptoms: Recurrence of fever, meningitis, kidney damage, liver failure, respiratory distress, and rarely, death.
Severe cases, known as Weil's disease, can involve jaundice, renal failure, haemorrhage, myocarditis, and pulmonary complications.
Diagnosis
Laboratory Tests: Serology (e.g., Microscopic Agglutination Test - MAT), PCR, culture, and enzyme-linked immunosorbent assay (ELISA).
Clinical Diagnosis: Based on symptoms and exposure history.
Treatment
Antibiotics: Penicillin, doxycycline, or azithromycin are commonly used.
Supportive Care: Includes hydration, pain management, and treatment of complications like renal or respiratory failure.
Prevention
Avoidance of Contaminated Water: Not swimming in or drinking from potentially contaminated sources.
Water Treatment: Water treatment is crucial in preventing leptospirosis, especially in areas where water sources may be contaminated by the urine of infected animals. Here are some effective water treatment methods to prevent leptospirosis:
1. Boiling
Process: Boiling water for at least one minute (or three minutes at higher altitudes) kills Leptospira bacteria.
Effectiveness: Highly effective, as heat inactivates the bacteria.
2. Chlorination
Process: Adding chlorine (sodium hypochlorite) to water. A typical dose is about 2-5 mg/L of chlorine.
Effectiveness: Effective against Leptospira if the water is clear. Turbid water may require pre-treatment to remove particles.
Considerations: Requires proper dosing and contact time (at least 30 minutes).
3. Filtration
Process: Using filters to remove bacteria and particulate matter from water.
Microfiltration: Removes particles larger than 0.1-10 microns.
Ultrafiltration: Removes particles larger than 0.01-0.1 microns.
Effectiveness: Effective if the filter pore size is small enough to remove bacteria. Ultrafiltration is more reliable for removing Leptospira.
Considerations: Regular maintenance and cleaning of filters are necessary.
Process: Exposing water to UV light (typically at a wavelength of 254 nm).
Effectiveness: Effective at inactivating Leptospira bacteria, provided the water is clear.
Considerations: UV systems require a reliable power source and regular maintenance.
5. Ozonation
Process: Treating water with ozone (O₃), a strong oxidizing agent.
Effectiveness: Highly effective at inactivating Leptospira and other pathogens.
Considerations: Requires specialized equipment and proper handling.
6. Solar Disinfection (SODIS)
Process: Using solar energy to disinfect water in clear plastic bottles exposed to direct sunlight for at least six hours.
Effectiveness: Effective against Leptospira in sunny climates.
Considerations: Works best in areas with strong sunlight and clear weather conditions.
7. Chemical Disinfection
Iodine or Chlorine Dioxide Tablets:
Process: Adding iodine or chlorine dioxide tablets to water.
Effectiveness: Effective against Leptospira if used according to instructions.
Considerations: Taste and potential health concerns with long-term use of iodine.
8. Coagulation and Sedimentation
Process: Adding coagulants (e.g., aluminum sulfate) to water to aggregate suspended particles, including bacteria, and then allowing them to settle.
Effectiveness: Improves water clarity and effectiveness of subsequent disinfection methods.
Considerations: Requires correct dosing and settling time.
Integrated Approach
Using a combination of methods can enhance effectiveness:
Pre-Treatment: Coagulation and sedimentation to remove larger particles and reduce turbidity.
Primary Treatment: Filtration to remove remaining particles and bacteria.
Secondary Treatment: Disinfection (chlorination, UV, or boiling) to ensure inactivation of pathogens.
General Considerations
Source Protection: Prevent contamination by protecting water sources from animal waste.
Regular Maintenance: Ensuring water treatment systems are properly maintained and functional.
Monitoring: Regular testing of water quality to ensure the absence of contaminants.
By implementing these water treatment methods, communities can significantly reduce the risk of leptospirosis and ensure safer drinking water.
Protective Clothing: For those working in high-risk occupations.
Rodent Control: Measures to reduce rodent populations.
Vaccination: Available for animals; human vaccines are used in some countries but are not widely available.
Public Health and Control Measures
Education and Awareness: Informing at-risk populations about transmission and preventive measures.
Surveillance: Monitoring outbreaks and reporting cases to health authorities.
Sanitation and Hygiene: Improving water and sanitation infrastructure to reduce contamination.
Prognosis
With prompt and appropriate treatment, the prognosis is generally good.
Without treatment, complications can be severe and sometimes fatal.
Research and Developments
Ongoing research focuses on better diagnostic methods, vaccine development, and understanding the mechanisms of pathogenesis and immunity.
Leptospirosis remains an important zoonotic disease with significant public health implications, especially in areas with poor sanitation and close human-animal contact.
As an Amazon Associate, I earn from qualifying purchases. This means that if you click on an Amazon link on this site and make a purchase, I may receive a small commission at no additional cost to you. This helps support the website and allows me to continue to provide content for you. Thank you for your support!
